Understanding Melanoma: A Simple Guide
Melanoma is a type of skin cancer that arises from the pigment-producing cells known as melanocytes. It is one of the most aggressive forms of skin cancer and can metastasize to other parts of the body if not detected and treated early. In this comprehensive guide, we will delve into the details of melanoma, covering its epidemiology, risk factors, pathophysiology, clinical presentation, diagnosis, staging, treatment options, prognosis, and prevention strategies.
Epidemiology:
Melanoma is relatively rare but is the deadliest form of skin cancer. Its incidence has been steadily increasing worldwide over the past few decades. According to the World Health Organization (WHO), there were an estimated 287,723 new cases of melanoma diagnosed globally in 2020, with 60,712 deaths attributed to the disease. The highest incidence rates are observed in regions with predominantly fair-skinned populations, such as Australia, New Zealand, North America, and Northern Europe.
Risk Factors:
Several factors can increase an individual's risk of developing melanoma. The primary risk factor is exposure to ultraviolet (UV) radiation from the sun or artificial sources like tanning beds. Other risk factors include:
1. Fair Skin:People with fair skin, light-colored eyes, and blonde or red hair are at higher risk due to decreased melanin production and less protection against UV radiation.
2. Sun Exposure:Prolonged exposure to sunlight, especially during peak hours (10 am to 4 pm), increases the risk of melanoma.
3. History of Sunburns: Severe sunburns, particularly during childhood or adolescence, elevate the risk of developing melanoma later in life.
4. Presence of Atypical Moles: Individuals with numerous moles or atypical (dysplastic) moles have a higher risk of melanoma.
5. Family History: A family history of melanoma or other skin cancers increases the likelihood of developing melanoma.
6. Weakened Immune System: Immunocompromised individuals, such as organ transplant recipients or those with HIV/AIDS, have an increased risk of melanoma.
7. Previous Melanoma: People with a history of melanoma are at higher risk of developing subsequent melanomas.
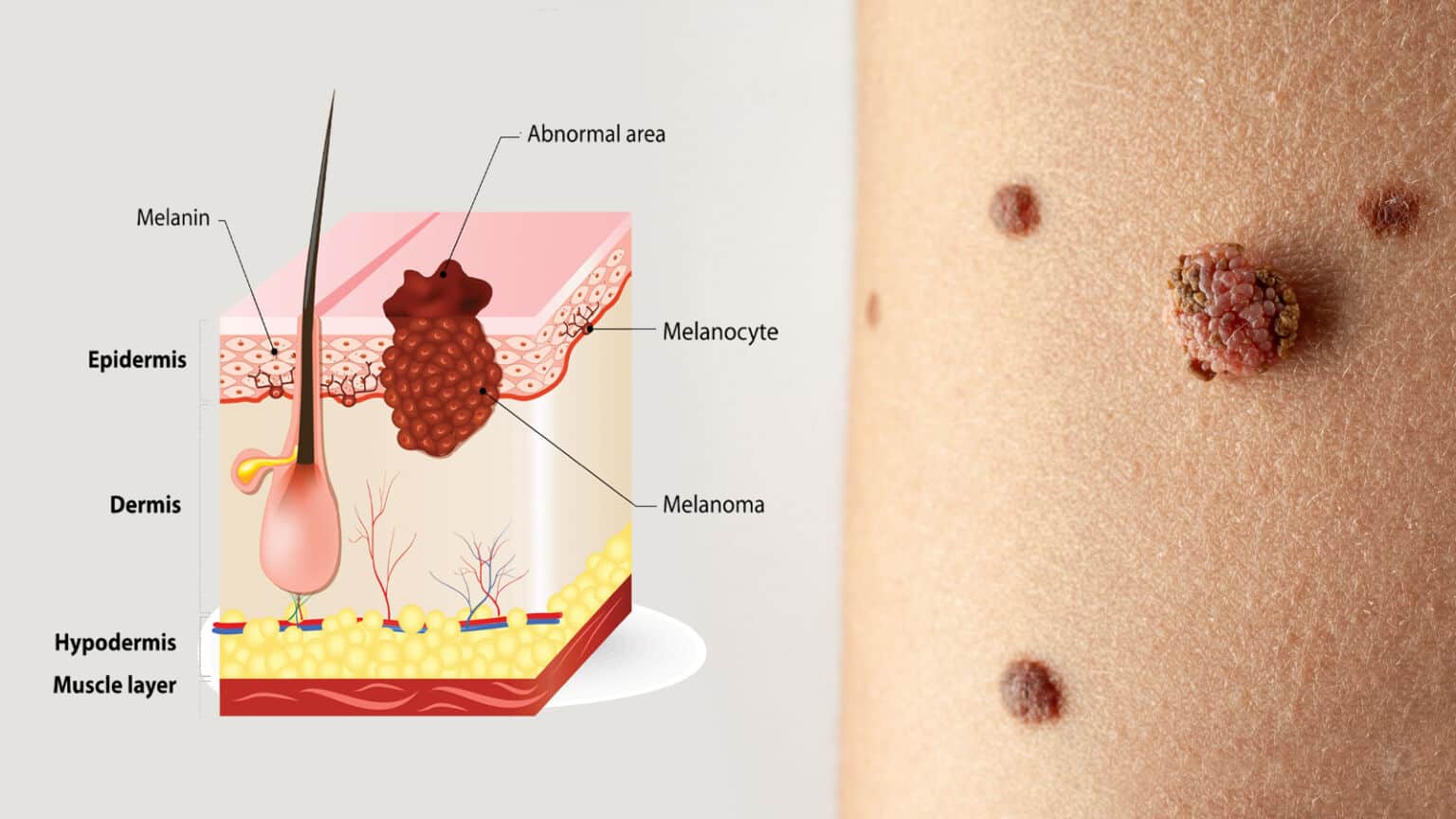
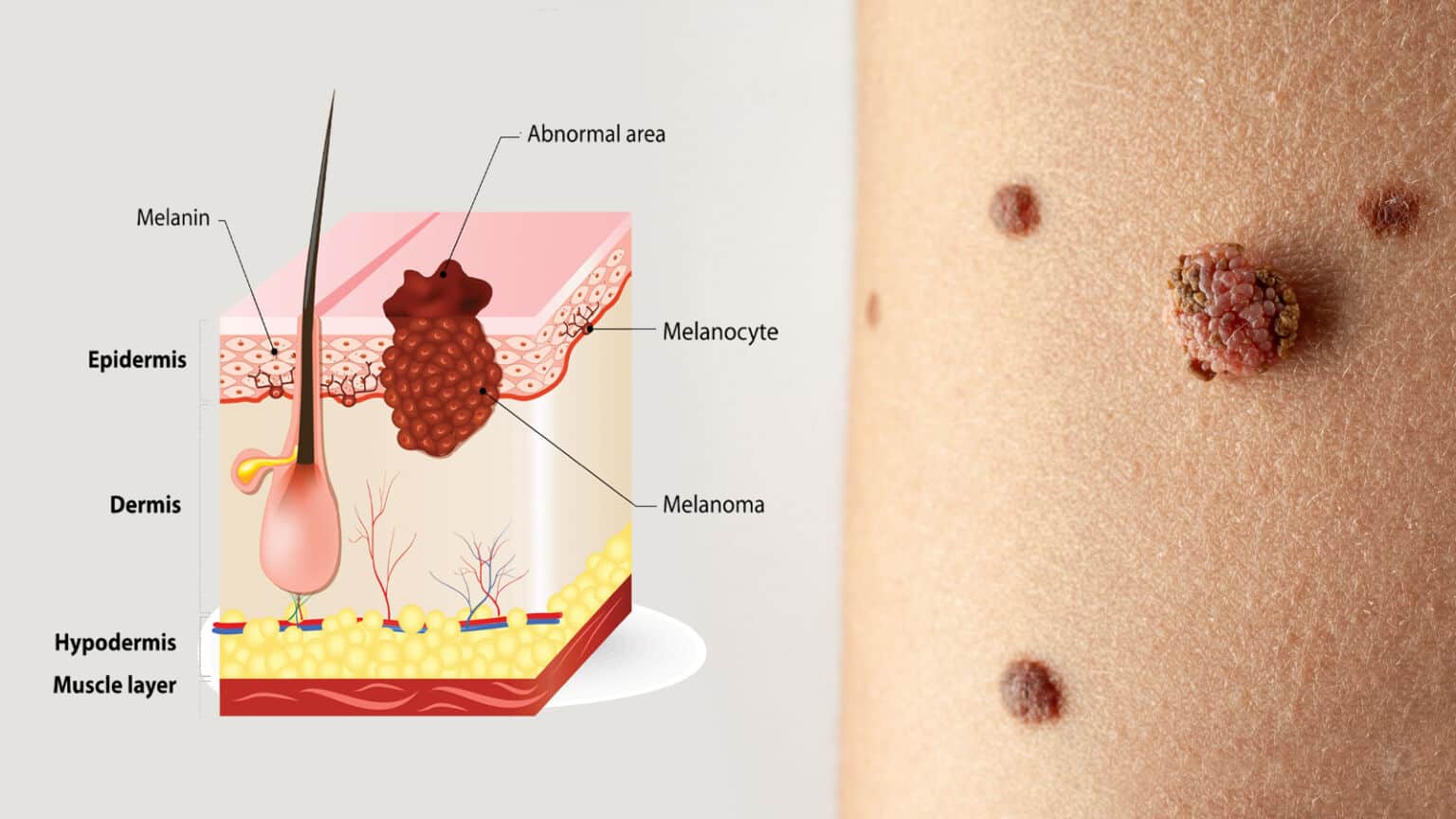
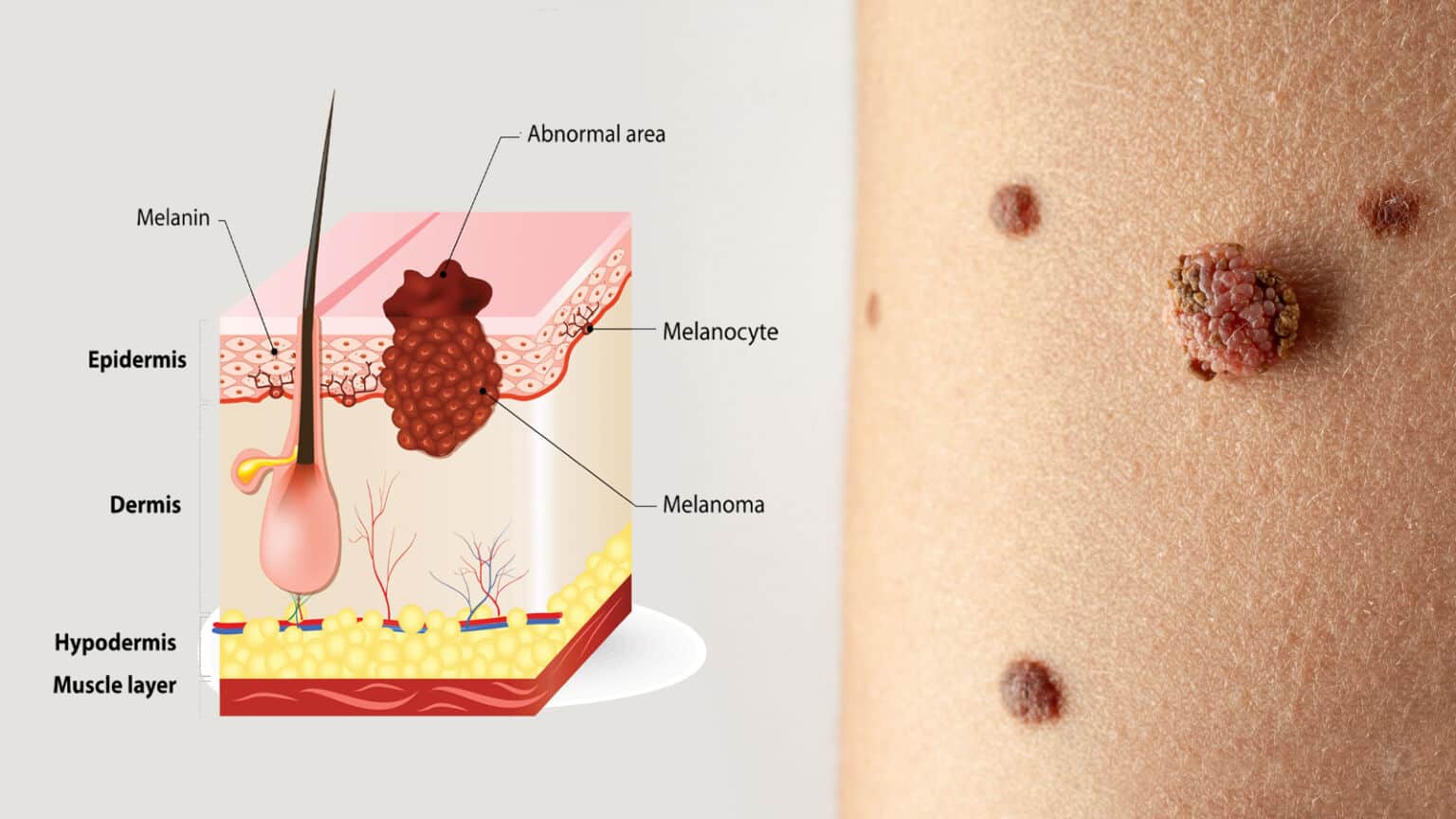
Pathophysiology:
Melanocytes are specialized cells located in the basal layer of the epidermis that produce melanin, the pigment responsible for skin color. Melanoma arises when melanocytes undergo malignant transformation, leading to uncontrolled growth and proliferation. The exact mechanisms underlying melanoma development are complex and involve both genetic and environmental factors. UV radiation is a major contributor to melanoma pathogenesis, causing DNA damage and mutations in key genes involved in cell cycle regulation and DNA repair pathways. Mutations in genes such as BRAF, NRAS, and CDKN2A are commonly found in melanoma tumors and play crucial roles in tumor initiation and progression.
Clinical Presentation:
Melanoma can present in various forms, but it typically appears as a new or changing mole on the skin. The ABCDE mnemonic can help in identifying suspicious features:
- Asymmetry: One half of the mole does not match the other half.
- Border Irregularity:The edges of the mole are ragged, notched, or blurred.
- Color Variation: The mole has multiple colors or uneven distribution of color.
- Diameter: The diameter of the mole is greater than 6 millimeters (about the size of a pencil eraser).
- EvolutionThe mole changes in size, shape, color, or other characteristics over time.
In addition to the ABCDE criteria, other signs of concern include itchiness, tenderness, bleeding, or the presence of a lesion that does not heal.
Diagnosis:
The diagnosis of melanoma is typically made through a combination of clinical examination, dermoscopy, and skin biopsy. Dermoscopy, also known as dermatoscopy or epiluminescence microscopy, is a non-invasive technique that allows for the magnified examination of skin lesions, aiding in the detection of subtle features suggestive of melanoma. If a lesion is deemed suspicious, a skin biopsy is performed to obtain a tissue sample for histopathological examination. The biopsy specimen is analyzed by a pathologist to confirm the diagnosis of melanoma and determine its characteristics, including tumor thickness, cell type, and presence of ulceration.
Staging:
Once melanoma is diagnosed, staging is performed to assess the extent of disease spread and guide treatment decisions. The most widely used staging system for melanoma is the American Joint Committee on Cancer (AJCC) TNM staging system, which considers tumor thickness, ulceration, lymph node involvement, and distant metastasis. The stages range from 0 (in situ melanoma) to IV (metastatic melanoma), with each stage having specific criteria and implications for prognosis and treatment.
Treatment Options:
The treatment of melanoma depends on several factors, including the stage of the disease, the patient's overall health, and individual preferences. Treatment modalities for melanoma may include:
1. Surgery: Surgical excision is the primary treatment for localized melanoma. The goal is to remove the tumor with adequate margins to ensure complete removal while preserving as much healthy tissue as possible. In cases of more advanced disease, lymph node dissection may be performed to remove affected lymph nodes.
2. Immunotherapy: Immunotherapy aims to harness the body's immune system to recognize and destroy cancer cells. Checkpoint inhibitors, such as pembrolizumab and nivolumab, target proteins that inhibit immune responses, allowing T cells to attack melanoma cells more effectively.
3. Targeted Therapy:Targeted therapy drugs are designed to interfere with specific molecular pathways involved in melanoma growth and survival. BRAF inhibitors, such as vemurafenib and dabrafenib, target mutated BRAF proteins commonly found in melanoma tumors.
4. Radiation Therapy: Radiation therapy may be used as adjuvant therapy after surgery to eliminate any remaining cancer cells or as palliative treatment to relieve symptoms in advanced-stage disease.
5. Chemotherapy:Traditional chemotherapy drugs may be used in the treatment of metastatic melanoma, although they are less commonly used today compared to targeted therapy and immunotherapy due to their lower efficacy and higher toxicity.
6. Combination Therapies: Some patients may benefit from combination therapies that involve a combination of immunotherapy, targeted therapy, or other treatment modalities. Clinical trials are ongoing to evaluate the efficacy and safety of various combination regimens.
Prognosis:
The prognosis for melanoma varies widely depending on several factors, including the stage of the disease, tumor characteristics, patient age, and overall health. Generally, early-stage melanomas (stages 0 to II) have a favorable prognosis, with high cure rates following surgical excision. In contrast, advanced-stage melanomas (stages III to IV) are associated with a poorer prognosis, as they are more likely to metastasize to distant organs and are less responsive to treatment. However, recent advancements in targeted therapy and immunotherapy have significantly improved outcomes for patients with metastatic melanoma, with some individuals achieving long-term remission or even cure.
Prevention:
Prevention strategies play a crucial role in reducing the risk of melanoma and other skin cancers. Key preventive measures include:
1. Sun Protection: Limiting sun exposure, especially during peak hours